Management of bleeding without transfusion of other people's blood.
The BEST and safest BLOOD for TRANSFUSION is your OWN BLOOD.
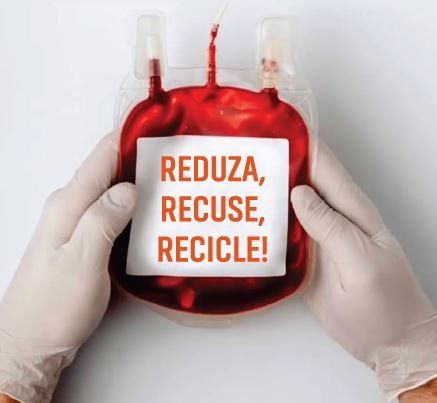
THE BEST BLOOD TRANSFUSION IS THE ONE YOU DIDN'T RECEIVE.
blood recovery machine
Cell Saver XTRA
BEST PRACTICES
OF AUTOTRANSFUSION
Acute nomovolemic hemodilution SAME DNA TRANSFUSION
Acute and hemorrhagic bleeding 10 STEPS TO SAVE LIVES
Systemic hemostasis and topical hemostasis COMPLETE ALGORITHM
PHARMACEUTICAL GUIDE TO HEMOSTATICS: DOSE, DILUTION, ROUTE OF ADMINISTRATION AND CONTRAINDICATIONS
BLEEDING MANAGEMENT PROTOCOL
Dr. Antonio Alcaeu dos Santos
Titular Member of the Brazilian Society of Cardiology
Dr. Luis Vicente Garcia
Titular Member of the Brazilian Society of Anesthesiology
Dr. Romilton Viana Machado
Titular Member of the Brazilian Society of Thoracic Surgery
The best, cheapest and safest blood for transfusion is your OWN BLOOD.
This blood has its trademark: its antigens, its antibodies, that is, a blood with its DNA. Therefore without any risk of immunological or inflammatory reaction.
How to achieve this?
Through a program WORLDWIDE known as PBM (Patient Blood Management), that is, a program for the conservation of the patient's own blood. Aiming at reducing the consumption of blood and its components, the World Health Organization (WHO) guides patient blood management (PBM) through three pillars: http://apps.who.int/gb/ebwha/pdf_files/WHA63 /A63_R12-en.pdf
First pillar: take all measures to optimize the patient's erythrocyte mass;
Second pillar: minimize the patient's blood loss;
Third pillar: optimizing, cooperating with each patient's physiological tolerance to anemia
The First Pillar concerns the treatment of any and all ANEMIA, with medications: ferrous sulfate or ferric hydroxide saccharate, folic acid, vitamin B12 and, when necessary, use erythropoietin, darbepoietin or CERA (continuous erythropoietin receptor activator). It is estimated that two billion individuals are anemic and that iron deficiency occurs in about four billion individuals around the world.
The Second Pillar is where we have the two main strategies that allow us to use the patient's own blood:
I - Intraoperative autotransfusion
Through an equipment/machine we are able to recover the patient's OWN BLOOD that would be lost during the surgery. As we said, this recovered blood has the patient's own DNA. It can be reused and does not represent a homotoxin (“foreign body”). When not recovered, it unfortunately goes to the garbage can along with gases and compresses. This is true blood recycling.
This recovery of red cells (red blood cells) during surgery is an excellent alternative to allogeneic (donated) blood, mainly due to the benefits, such as: immediate availability of fresh blood, reduction of postoperative complications, reduction of the number of hospitalization days and associated infections, reduced death, as well as decreased demand for homologous blood (bags).
The cost of this procedure is approximately the same price as one to two bags of blood, when considering all the activities involved in blood transfusion.
II – Acute Normovolemic Hemodilution
This is one of the simplest and cheapest treatment options for using your OWN BLOOD in surgery. It consists of removing one, two, three or more bags of blood from the patient at the beginning of the surgery, being replaced by crystalloid and/or colloid solutions as plasma volume expanders, to maintain normovolaemia (circulating volume). This blood will be available to the surgeon to be used at the appropriate time, usually at the end of the surgery. If there is any bleeding in the surgery, we will have less blood loss, since it will be more diluted. This stored blood has the patient's DNA, with no risk of immunological reactions. The cost of this procedure is approximately U$20.00 (twenty dollars) or R$70.00 (seventy reais), which would be the cost of two empty blood collection bags. This blood can be purified in the XTRA autotransfusion device to be purified and thus sent back to the patient.
The Third Pillar is one of the main pillars of the PBM program.
THE BEST BLOOD TRANSFUSION IS THE ONE YOU DIDN'T RECEIVE.
Research shows that humans tolerate/support critical levels of anemia. On the other hand, the transfusional medical practice sometimes reaches 100% in several hospitals, mainly in cardiac surgery. PATIENT tolerates anemia, DOCTOR does not tolerate anemia.
WHO recognizes that the safety of patients transfused with allogeneic (donated) blood is seriously compromised by the excessive and unnecessary use of blood, plasma and derivatives transfusions, unsafe transfusions and transfusion errors (especially at the patient's bedside).
Concerned about the risks related to the traditional transfusion practice, performed with donation bags, the WHO strongly encourages the creation of a patient's own blood conservation program (PBM). In the last decade, the veracity of these facts is increasingly evident by scientific research published by several national and international researchers.
To conclude, the WHO itself recommends “…reduce unnecessary transfusions to minimize the risks associated with transfusion; use alternatives to transfusion whenever possible, and good and safe clinical transfusion practice includes managing the patient's blood.” World Health Organization. Safety and availability of blood. Revised June 2015. http://www.who.int/mediacentre/factsheets/fs279/en/
Therefore, it is important to make known the main treatment options for transfusions to save blood components, which are already scarce in blood banks. As evidence from the real world.
When there is the purpose and multiprofessional involvement, of the clinician, the surgeon, the anesthesiologist and/or the intensive care physician, to manage and conserve the blood of autotransfusion (the person's own blood) it is possible to perform small, medium, severe and complex without the use of another person's blood (allogeneic).
The BEST and safest BLOOD for TRANSFUSION is your OWN BLOOD.
THE BEST BLOOD TRANSFUSION IS THE ONE THAT DIDN'T RECEIVE
The video below is a class on clinical and surgical strategies that reduce blood transfusions based on PBM principles, taught by Professor Dr. Antonio Alceu dos Santos, cardiologist, PhD in hematology, member of SABM (Society for the Advancement of Blood Management), specialist in the Brazilian Society of Cardiology and Brazilian Medical Association.






